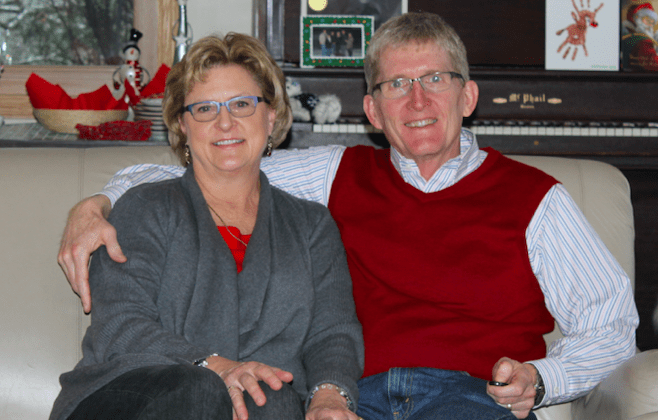
Carole shared her story in April of 2019.
Thinking of end-of-life care issues went from an abstract thought to very real, urgent concerns for me and my husband, Jim, when he was diagnosed with stage 4 terminal melanoma and bowel tumors in August of 2015. The cancer had already spread to his hip and required hip replacement surgery. Fortunately, he recovered well from that surgery and the immunotherapy treatments he received worked for a couple of months, but by the beginning of 2016 they had stopped working.
Doctors recommended Jim try surgery to manage his cancer, however, surgery failed and then chemotherapy was offered. Jim faced the hard decision of receiving chemotherapy that would have harsh side effects or stop all treatment. He decided to discontinue all treatments and focus on his quality of life.
Prior to Jim’s illness, we had had conversations about medical aid in dying and we both felt it was an important, compassionate end-of-life care option, not imagining we would one day potentially need the option for ourselves. We, however, were never willing to consider moving out of state to become eligible to use such laws. Moving would have meant being away from friends and family, and that would have been a terrible hardship on us both.
Knowing that we were unwilling to move to access medical aid in dying, Jim opted for in-home hospice care. We were promised comfort care at home; and in our minds, hospice would be able to relieve Jim’s pain and symptoms. Sadly, no matter what is done, sometimes hospice can not make everyone comfortable.
Jim’s pain could not be managed at home, so we were sent back to the hospital by ambulance, for pain management. Once his pain was under control after re-hospitalization, we chose to go to a hospice facility rather than receive home hospice care because we were reassured that all the medications Jim might need to keep him comfortable would be on site, for immediate administration as needed.
Jim’s primary concern at the end of his life was that he would be kept comfortable, which he communicated to me and outlined in his POLST. He feared being in pain in his last weeks. Hospice, unfortunately, was unable to provide immediate comfort care. Jim was grimacing, moaning, saying, “Help me.”
I am left with anger, remorse, and sadness for what Jim went through and my feeling of failure that I couldn’t make sure he had the comfort care which had been promised to him. Hospice is a wonderful option for most, but there are some people whose pain and symptoms simply cannot be managed. It was horrific watching the one I love suffer.
There is a need for more end-of-life options in Minnesota. I ask legislators to imagine someone that they love very deeply suffering in the manner my husband did. Medical aid in dying would provide another palliative option and could prevent prolonged, painful deaths like my husband’s.