Oliver shared his story in May of 2023.
When I was 10 years old, my mother moved us to Illinois from Georgia to get away from picking cotton. It was the late 1950s. My mother took on three domestic jobs here in Evanston so that we did not have to be raised amidst the hardships of sharecropping like she had done.
Of course, one great tragedy is that while my mother fled the Jim Crow South to give us a better life, racial inequities would continue to bear down on the lives of Black people, like me here in Illinois. They still do, 65 years after I came here — I saw it when my mother died, and I’ve seen it through my own bouts with cancer, particularly in the ongoing lack of access for the Black community to information about end-of-life healthcare and options. Although I could never pay back my mother for her sacrifice, in some ways the driving force for my life has become trying to repay her by helping other people get the information they need.
I’m an educator by profession and at heart. I retired after 36 years as a teacher, assistant principal and principal. After that, I worked for 12 additional years as an administrator. But when it comes to end-of-life care and planning, my own education didn’t come until 2001, at my mother’s deathbed.
I was with my mother at the hospital the last hours before she passed. She had a tube inserted down her throat, and when medical staff came in to suction congestion out of her system, blood was coming from her mouth. I was alarmed, unaware that this is a normal occurrence when someone is near the end of life. I didn’t understand a number of things about death. It was a challenging situation because my mother and I hadn’t really planned for the end. I also didn’t know what all could be done to make her comfortable.
Immediately after she died, I was also faced with the neglect African American people often experience in healthcare systems when the hospital delayed the release of her body for reasons that were never made clear to me. By the time my mother’s body was released, she was swollen and disfigured. I had to afford the expenses of an autopsy for some informational clarification.
These experiences made me question the attentiveness of the medical staff at the hospital. It was very disheartening how they had treated my mother. The end of her life felt out of step with the dignity and respect she deserved.
Four years later I retired, and shortly thereafter I learned I had prostate cancer. Given the choice of radiation, chemotherapy or surgery, I chose surgery. It went well. The doctor informed me that despite the procedure’s success, however, the cells were likely to regrow.
I went years with no evidence of disease. Then, in 2022, my wife and I developed COVID.
I started having ongoing pain that I couldn’t get rid of. My wife urged me to go to the doctor, but I didn’t want anyone to worry. Then one morning the pain hit me like an 18-wheeler truck, so excruciating that I finally decided to go to the hospital.
When we got to the hospital, the medical staff saw my distress and immediately called me back for a CAT scan, MRI and other examinations. After about an hour, the doctor said, “I’ve got some news. And it’s not the best of news. Had you been five minutes later, you would not have made it.” Not only had my appendix ruptured, causing sepsis to set in, but the doctors had also observed a mass behind the wall of my appendix.
Over the next six days, they drained the fluids from my system; three weeks after I had come in, they performed surgery to remove the mass. It was colon cancer. Luckily, as before, this surgery was a success, and the doctor informed me that the good news was I wouldn’t have to have radiation, chemo or a colostomy bag.
My health episodes, along with my mother’s death, have given me a new perspective on preparing for the end of life. I’ve been involved with Compassion & Choices for years now, after an acquaintance I met at Northwestern University’s Osher Lifelong Learning Institute urged me to attend a meeting. At first I wondered, “Why is she inviting me? Do I look like I’m going to die?” But then I actually went to a meeting and found the information to be incredibly helpful. Learning about end-of-life planning and options has helped me start preparing for my own demise, doing things that will hopefully make the situation easier for my wife and daughters so they don’t have to go through what I went through with my mother.
At the end of my life, I want there to be harmony and closure for me and my family. I don’t want there to be disorganization or confusion. And I’d like to have the full range of end-of-life care options provided — including the option of medical aid in dying — so that I can say my goodbyes in a way that allows my family to move on.
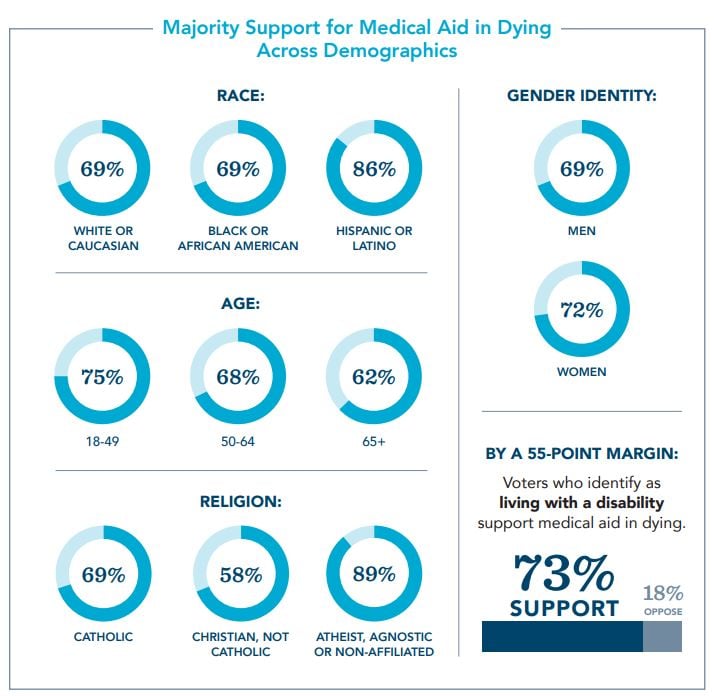
I feel that I have a responsibility to provide information about the option of medical aid in dying to my community. A variety of life circumstances prevented me from having information about end-of-life care options like medical aid in dying for a long time, but now I’ve seen how much it would have been helpful for me to have more information. It would have helped me be better prepared. I describe being exposed to the existence of this option as itself educational. In fact, the evidence shows that medical aid-in-dying laws actually increase education about all available end-of-life options, including palliative and hospice care, because they spur conversations about end-of-life care between terminally ill people, their doctors and their loved ones.
A medical aid-in-dying law in Illinois would give terminally ill people more choices and one way to make their final moments as meaningful as they can be for themselves and their loved ones. When it comes to healthcare, Black Americans don’t always get the same options as white people. But having more information and increased preparation allows us to be the beneficiaries of some of those opportunities.
God gives us choices throughout our lives, and I believe his will is done through us and the choices we make. I trust that however I get to the end of my life will be God’s will for me. The thing about medical aid in dying is that it is an option that can help people who need it if they choose to use it — nothing more or less.

 For Patients Access the Illinois Advance Directive
For Patients Access the Illinois Advance Directive
 End-of-Life Planning Use our step-by-step guide to chart your journey.
End-of-Life Planning Use our step-by-step guide to chart your journey.
 Los recursos en Español Los recursos en Español.
Los recursos en Español Los recursos en Español.
 COVID-19 Toolkit Get answers to your questions about COVID-19
and end of life care.
COVID-19 Toolkit Get answers to your questions about COVID-19
and end of life care.
 Resources for Providers Find resources tailored to the needs of healthcare providers.
Resources for Providers Find resources tailored to the needs of healthcare providers. 


